At the other end of the life spectrum, assisted suicide teaches that some lives are more valuable than others. It’s a tragic failure of our culture by violating human dignity at its deepest level and advancing the fatal idea of a “final solution” that “relieves” society of its duty to provide compassionate care to vulnerable citizens.
This dangerous ideology affects the elderly, the vulnerable, the disabled, and those with limited financial resources. Legalizing assisted suicide only “helps” people who are no longer responsible for the people who fall into these categories.
Heartbreakingly, research shows that most people who seek assisted suicide do so because they fear being a burden to their loved ones. As an organization that supports life-affirming policies, Kansas Family Voice stands against assisted suicide and supports policies that encourage holistic palliative care for people at the end of their lives. We also support legislation ensuring patients have faster access to experimental drug treatments.

ASSISTED SUICIDE LAWS EXPLAINED
Assisted suicide laws give doctors the legal right to prescribe life-ending drugs to patients who have been diagnosed with a terminal illness and request help to end their life. Deceptively named by proponents as Death with Dignity, End of Life Options, or Compassionate Care, assisted suicide is anything but dignified or compassionate, and leaves the patient few options.
In America, lethal pills are prescribed by a physician requiring the patient to take them on their own, which is why it is called physician-assisted suicide. Alternatively, in Europe the term euthanasia is used as the physician directly administers life-ending drugs into the patient.
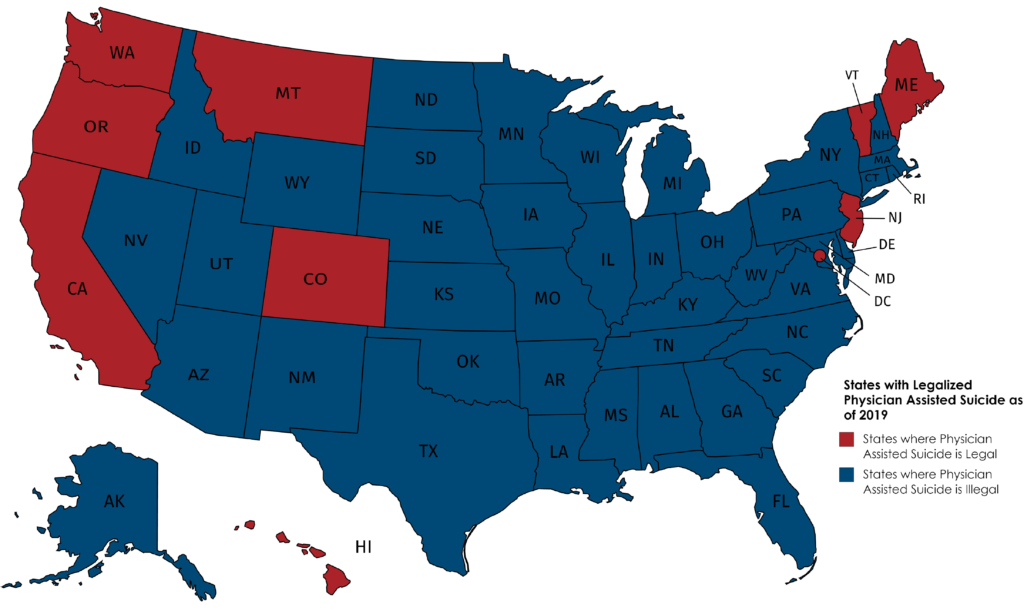
Oregon was the first state to legalize physician-assisted suicide in 1997. Maine and New Jersey were the most recent states to legalize assisted suicide in 2019, bringing the total number of states that allow the practice to nine. In those nine states, the assisted suicide laws are very similar. Most of the laws:
- Require a doctor to prescribe the medication
- Require a patient to have 6 months or less to live1
- Require a prescription for the life-ending medication
- Require the patient be a resident of the state
- Require the patient to be 18 or older
- Permit physicians to falsify death certificates2
In the past few years, 10 state legislatures have considered laws that would legalize assisted suicide. Despite those efforts, today, 39 states have laws expressly prohibiting assisted suicide, and more than half have defeated legislation attempting to legalize it. Even the Supreme Court has ruled that there is no inherent constitutional right to assisted suicide in our nation, as the practice is offensive to our national traditions and practices.
ASSISTED SUICIDE REMAINS A CRIMINAL OFFENSE IN 41 STATES
1 Life expectancy is always an estimate. There are many cases of a patient living beyond the speculated date.
2 The cause of death is listed as the underlying illness, rather than assisted suicide.
THE IMPACT OF LEGALIZING DEATH
DOCTORS AREN’T HEALERS WHEN PRESCRIBING DEATH
“Physician-assisted suicide is fundamentally incompatible with the physician’s role as healer, would be difficult or impossible to control, and would pose serious societal risks.”1
This is the current position of America’s largest physician association, the American Medical Association. Many have long associated the ancient phrase “first, do no harm” from the Hippocratic Oath all doctors take with medical practice worldwide. For thousands of years, the cornerstone of the medical profession has been to offer healing. Assisted suicide is not only unethical but opposed to the very profession of medicine and is ultimately harmful to the physician’s ability to provide authentic compassionate care.
Kansas Family Voice honors the historic role of doctors as healers and supports policies that allow doctors to fulfill their mission through adequate comfort care and pain control.

INSURANCE PROFITING FROM CHOOSING DEATH
There is a significant problem in America when large insurance companies and HMO’s can save a substantial amount by ensuring their sickest patients are able to end their lives prematurely. The average cost of lethal medication is $300, and most insurance companies will cover well over 90% of that cost — leaving copays around $5 or less! Yet, the cost of treatments for the underlying conditions, such as for chemotherapy, is far greater, potentially reaching hundreds of thousands of dollars.
The impact of this price difference is that people who are economically disadvantaged are far more vulnerable to pressures to choose suicide drugs instead of continuing treatment. These populations are particularly sensitive to concerns about becoming burdens to their families or racking up massive debt. There have been cases of insurance companies refusing to cover treatment options and experimental drugs for patients who want to live but offering instead to cover assisted-suicide drugs.
PARTICIPATING IN DEATH THREATENS LIBERTY
Religious associations in America, like Catholic hospitals, have emphatically opposed Assisted Suicide as utterly incompatible with not only their faith-based missions but also their very reason for existence: to carry out the love of Christ through medical care that values every person’s life.2 Kansas Family Voice advocates for the conscience and faith rights of physicians and other medical professionals so that that they never find themselves in a situation where they are compelled to assist anyone in the act of suicide, no matter the reason.
Kansas Family Voice applauds the Trump Administration’s new rule3 ensuring that doctors’ rights of conscience are protected.4 Doctors will freely be able to decline to provide or participate in providing assisted-suicide drugs or even inform or counsel a patient that these drugs are available. This conscience-protection rule also allows insurance companies to decline coverage for assisted-suicide drugs.
A DOCTOR SHARES WHY ASSISTED SUICIDE VIOLATES “FIRST, DO NO HARM”
1Opinion 5.7 Physician-Assisted Suicide. American Medical Association. Code of Medical Ethics https://www.ama-assn.org/delivering-care/ethics/physician-assisted-suicide
2See e.g. https://www.centura.org/locations/penrose-st-francis-health-services/about
3https://www.hhs.gov/sites/default/files/final-conscience-rule.pdf
4This rule applies to Medicaid and Medicare providers, hospitals, nursing facilities, home health or personal care service providers, hospice programs, Medicaid managed care, health maintenance organizations,Medicare+Choice/Advantage org’s and prepaid org’s.
PROTECTING THE VULNERABLE
When a society, which is supposed to protect the vulnerable, begins to advocate for their death, that must be a wake-up call for us to see assisted suicide for its truly dark, treacherous nature.

PHYSICAL DISABILITIES
The majority of people requesting assisted suicide are doing so not because of pain, but for fear of being a burden to loved ones through increasing disability and loss of autonomy.1 Sadly, assisted-suicide proponents ultimately use that fear to legalize a pathway for people to end their lives. Yet, disability-rights advocates have spent decades teaching and raising awareness that loss of autonomy is not undignified or to be feared as a type of “living death.” They have demonstrated that every life is valuable and priceless — every life is worth fighting for.

MENTAL HEALTH CONDITIONS
Recently, some European countries that have legalized euthanasia have been providing lethal injections to people with no physical terminal illness at all, but to people with schizophrenia, autism, bipolar disorder, dementia, and depression. These people were not dying. They were simply given a “final solution” to their severe psychological struggles. There’s a word for this type of “treatment” — murder. Assisted suicide is an irreversible and unacceptable solution to problems that can be treated with comprehensive mental health care.

CHILDREN
In 2014, Belgium expanded its euthanasia laws to include children of any age. Since that time, at least three children have died after receiving lethal injections at the “child’s request.” The Netherlands allows assisted suicide for children over 12.2 And Canadian hospitals have begun to advocate for children to have the right to choose whether or not they want to end their own lives,3 without parental consent or even parental notification. Learn more about Parental Rights
KANSAS FAMILY VOICE SUPPORTS INCREASED ACCESS TO PALLIATIVE CARE, IN-HOME SUPPORT OPTIONS, AND ACCESS TO EXPERIMENTAL AND MENTAL HEALTH TREATMENT.
1 https://dredf.org/public-policy/assisted-suicide/why-assisted-suicide-must-not-be-legalized/
2 https://www.washingtonpost.com/opinions/children-are-being-euthanized-in-belgium/2018/08/06/9473bac2-9988-11e8-b60b-1c897f17e185_story.html?utm_term=.981b10d9f8fc
3 https://www.catholicregister.org/item/28133-assisted-suicide-plans-for-children-unveiled-at-toronto-s-sick-kids-hospital
LACK OF ASSISTED SAFEGUARDS IN SUICIDE LAWS
Proponents of assisted suicide offer four “safeguards” to protect vulnerable patients.
Yet, none of these “safeguards” provides real protection.
The patient must request the lethal drugs in writing from a physician.
The requirement to request the drugs from a physician simply leads to “physician shopping” to find a doctor who is willing to sign off on the request if the patient’s own doctor — who is likely more familiar with the patient, the patient’s condition, and the patient’s mental state — declines for professional or moral reasons.
The request must be voluntary.
The “voluntary written request” requires a signature by the patient and often must be witnessed by two people, one of whom can be a financial heir. In America, if a witness to the signing of a will is an heir, there is a legal presumption of possible coercion and fraud. Yet, if an heir is a witness to a signature for suicide drugs, there is no such presumption, leaving very ill patients vulnerable to coercion and abuse by heirs.
The patient must be terminally ill, with a prognosis of six months or less to live.
The law requiring patients only have six months to live is also not a sufficient safeguard because physicians simply cannot predict how much time an individual patient has left to live. Such prognoses are never based upon the individual patient’s condition and are notoriously unreliable and inaccurate.1
The patient must self-administer the drugs.
Once a patient picks up their prescription from the pharmacy, there is no follow-up or oversight as to what happens to the lethal medication. There is no real way of knowing whether the patient took it of their own free will, how the patient took it, or whether the lethal dose was safely disposed of if the patient did not take it.
Kansas Family Voice has even seen a shift to make these so-called “protections” even weaker. In early 2019, New Mexico proposed legislation that did not require that a patient request their doctor discuss suicide drugs with them. This means that the doctor could suggest the patient consider the drugs herself, without the patient ever having raised the topic voluntarily first. The legislation didn’t even require a physician to prescribe the drugs but would have allowed nurses and physician assistants to do so. Finally, it also did not require a six-month approximate prognosis, but only that death would result in the ambiguous “foreseeable future.”
WATCH ELIZABETH’S STORY OF FACING A TERMINAL PROGNOSIS.
1 E.B. Lamont et al., “Some elements of prognosis in terminal cancer,” Oncology (Huntington), Vol. 9, August 13, 1999, pp. 1165-70; M. Maltoni, et al., “Clinical prediction of survival is more accurate than the Karnofsky performance status in estimating lifespan of terminally-ill cancer patients,” European Journal of Cancer, Vol. 30A, Num. 6, 1994, pp. 764-6; N.A. Christakis and T.J. Iwashyna, “Attitude and Self-Reported Practice Regarding Prognostication in a National Sample of Internists,” Archives of Internal Medicine, Vol. 158, Num. 21 November 23, 1998, pp. 2389-95; J. Lynn et al., “Prognoses of seriously ill hospitalized patients on the days before death: implications for patient care and public policy,” New Horizons, Vol. 5, Num. 1, February 1997, pp. 56-61. Also: “17 percent of patients [outlived their prognosis] in the Christakis study. This roughly coincides with data collected by the National Hospice and Palliative Care Organization, which in 2007 showed that 13 percent of hospice patients around the country outlived their six-month prognoses. … When a group of researchers looked specifically at patients with three chronic conditions—pulmonary disease, heart failure, and severe liver disease—they found that many more people outlived their prognosis than in the Christakis study. Fully 70 percent of the 900 patients eligible for hospice care lived longer than six months, according to a 1999 paper published in the Journal of the American Medical Association.” See Nina Shapiro, “Terminal Uncertainty,” Seattle Weekly, January 14, 2009, available at http://www.seattleweekly.com/content/printVersion/553991/ (accessed July 13, 2009)
SPEAK UP
We have the right, privilege and obligation to speak into every aspect of our government. Our Action Center makes it easy for you to do that.